What is endocarditis?
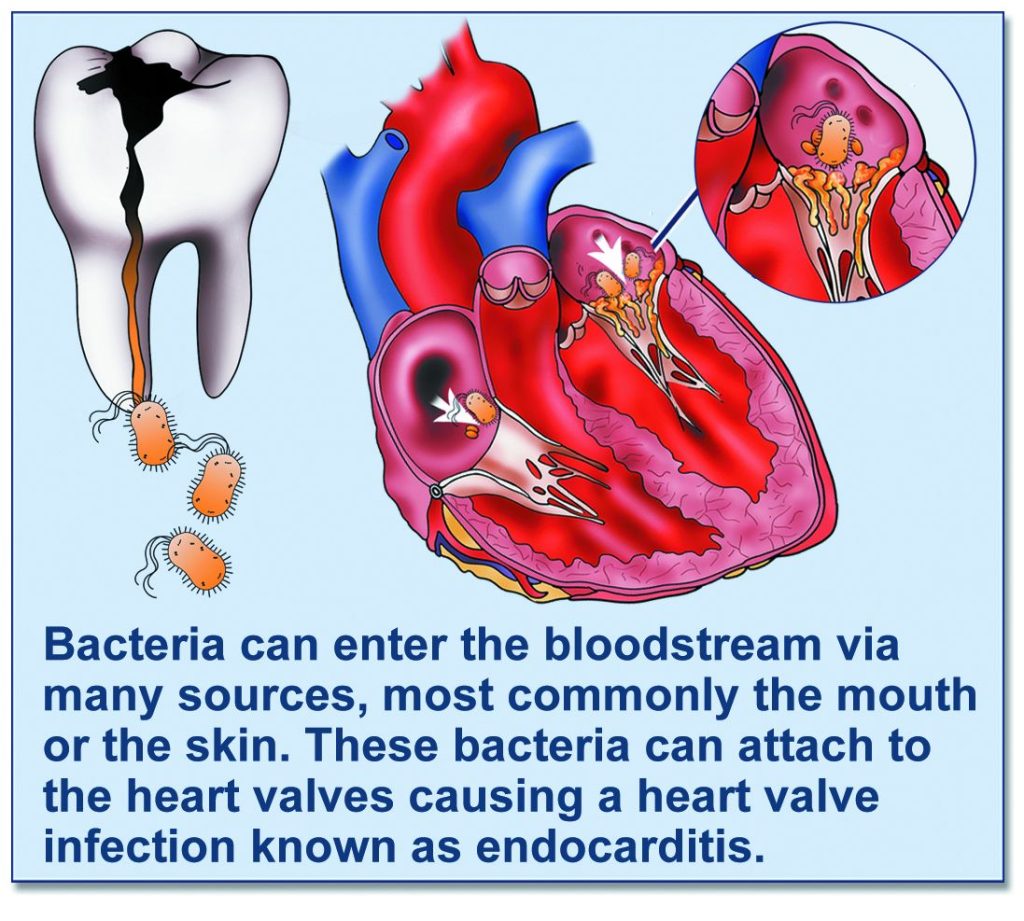
Endocarditis is a rare but potentially life-threatening infection of the lining of the heart. It usually affects the heart valves. It affects around 1 person in every 10,000 per year.
It is caused by bacteria entering the bloodstream, (usually via the mouth or the skin). Most of these bacteria are killed by the immune system but occasionally they can attach to the heart valves and cause you to become unwell.
Who is at increased risk of developing endocarditis?
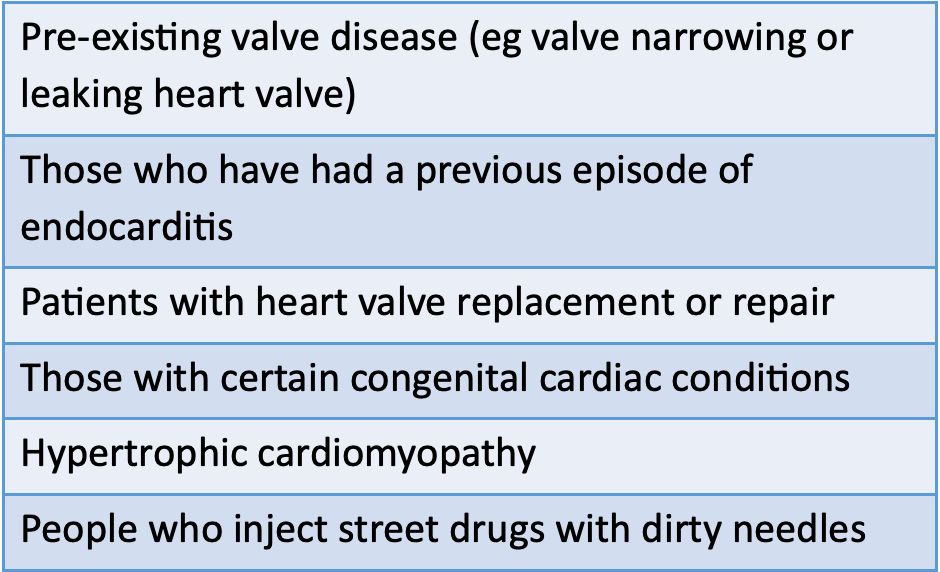
Although it is possible for anyone to develop endocarditis, the risks are increased in those with certain cardiac conditions including:
What can I do if I am at risk of endocarditis?
If you are at risk of endocarditis it is important that you take measures to reduce your risk of bloodstream infection.
Teeth
Take good care of your teeth by brushing twice a day and visiting your dentist for regular check-ups (at least once per year). If you have toothache or an abscess it is really important that you get treated for this quickly. Be sure to tell your dentist you have a heart condition.
Skin
Keep your skin clean by washing regularly. Wash any cuts and grazes and keep them clean until they heal.
If you notice that the skin becomes red and inflamed, tender to touch or there is a discharge then see your GP as you may have developed a skin infection. If your GP feels that you have a skin infection, they may prescribe antibiotics.
Any cosmetic procedures that involve breaking the skin such as tattoos, fillers, Botox and piercings will also give you an increased risk of endocarditis and therefore should be avoided.
Who is at the ‘highest risk’ of developing endocarditis?
Certain groups of patients are considered ‘higher risk’ of developing endocarditis, although it is important to remember that even if you are in this category, endocarditis is still a rare disease:
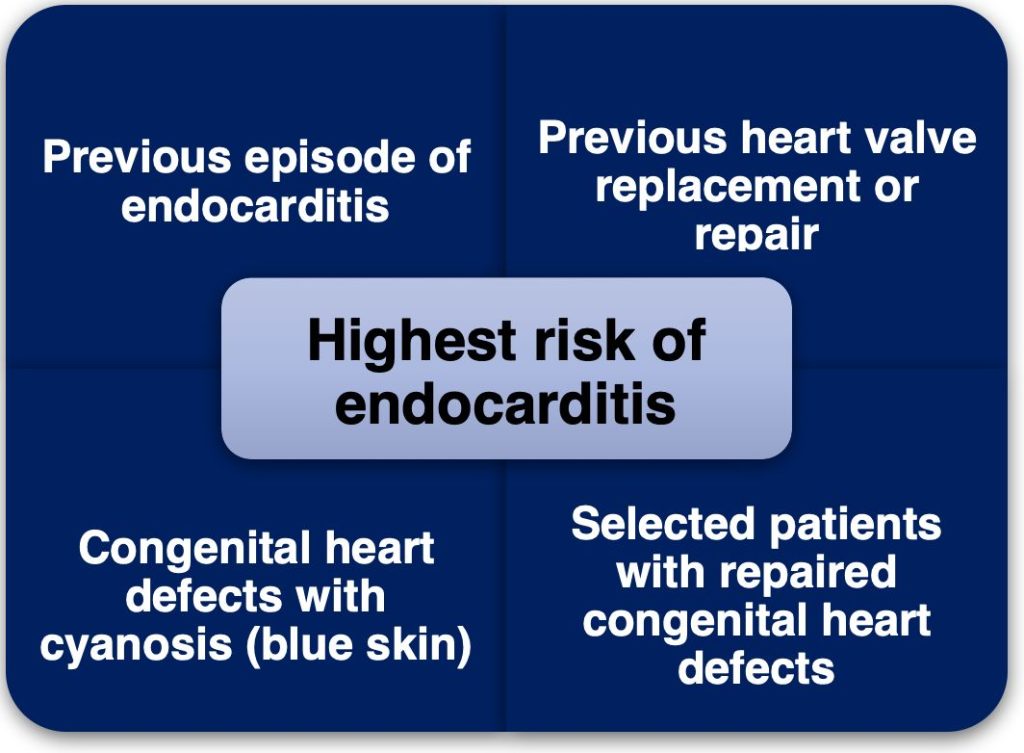
What does it mean if I am in the ‘highest risk’ category of endocarditis?
Patients who are considered to be ‘highest risk’ for endocarditis may be considered for antibiotics prior to certain dental treatments to reduce the risk of heart valve infection.
If you are considered to be at ‘highest risk’ of endocarditis, your Healthcare Professional will let you know and you should tell your dentist about this prior to any dental treatment. Your dentist will discuss the pros and cons of taking antibiotics.
Antibiotics can commonly cause nausea and diarrhoea. Rarely they can cause allergic reactions, bowel inflammation (colitis) and antibiotic resistance.
The decision regarding whether you should take antibiotics will be made between you and your dentist.
‘The best way of preventing endocarditis is by maintaining good dental hygiene, rather than antibiotics’
If you decide to take antibiotics prior to dental treatment then you will be prescribed
- A single dose of amoxicillin (3 grams) to be taken 60 minutes prior to the procedure
- If you have a penicillin allergy, 600mg clindamycin to be taken 60 minutes prior to the procedure.
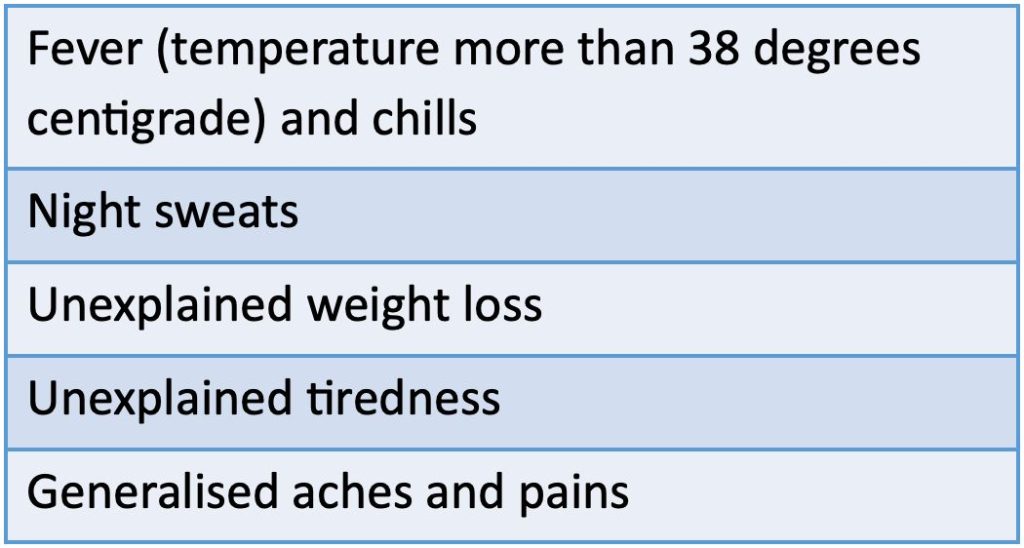
What are the symptoms of endocarditis?
The symptoms of endocarditis are vague and this can make it difficult to diagnose. Some symptoms of endocarditis are outlined below. As endocarditis is very rare, it is still unlikely that you have endocarditis even if you have these symptoms:
What do I do if I think I have endocarditis?
See your GP as soon as possible. Explain you are at risk of endocarditis and describe your symptoms. Your GP may wish to perform some blood tests. If they are also concerned that you may have endocarditis then they may refer you to the hospital for further investigation.
It will also be helpful for you to take your temperature when you feel you have a fever. Write the temperature measurements down and take them to your GP
