
The new ESC guidelines on the management of endocarditis were published this month in the European Heart Journal. These replace the previous iteration of the guidelines published in 2015 and provide important updates including an increasing recognition of the role of cross-sectional imaging as an adjunct to echocardiography, changed guidance to prevention of device infections, and strengthened recommendations regarding antibiotic prophylaxis. The guidelines reflect the demographic of the disease changing, with an increased number of device related infections and emergence of streptococcal antibiotic resistance.
The guidelines represent a comprehensive and inclusive document which are worthy of extensive review by all those involved in the management of endocarditis; however, highlights include:
Antibiotic prophylaxis is now recommended for all those with previous endocarditis, surgically implanted valves / previous repair and TAVI/ percutaneous pulmonary valves. These recommendations have been upgraded from IIa in 2015 to class I. New guidance is issued recommending antibiotic prophylaxis in those with ventricular assist devices (class I recommendation) and heart transplant recipients (class IIb). Mitral and tricuspid clips should have antibiotic prophylaxis considered as a class IIa recommendation.
All patients should be discussed with the Endocarditis team, with complex IE patients being managed in a cardiac surgical centre with endocarditis expertise as a class I indication (upgraded from IIa recommendation on previous guidance).
Cardiac CT and [18F]FDG-PET/CT are now a class I indication to detect valvular lesions in prosthetic valve endocarditis. Brain and whole-body imaging is also now a class 1 recommendation in patients with both symptomatic prosthetic and native endocarditis to detect peripheral lesions or add minor diagnostic criteria, with a class IIb recommendation in asymptomatic patients. CT should also be used (especially if echo is inconclusive) to detect perivalvular and periprosthetic complications of IE including abscesses, pseudoaneurysms and fistulae.
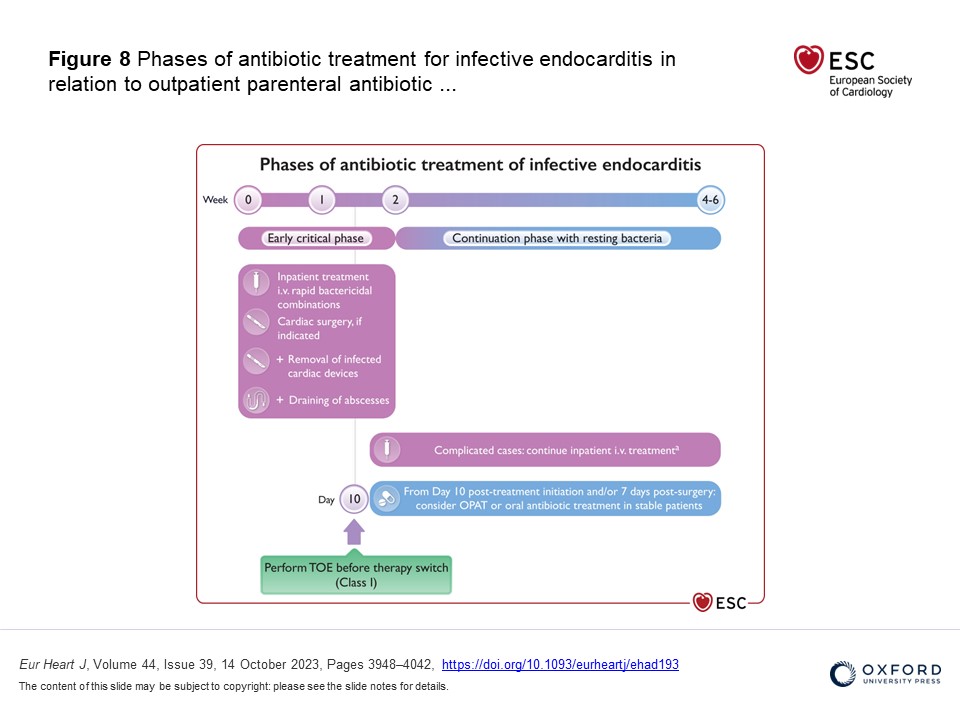
Out-patient parenteral antibiotic treatment (OPAT) (or in selected cases oral antibiotic treatment) is recommended in the guidelines now for clinically stable patients with left sided IE without severe valve disease or abscess caused by Streptococcal spp, Enteroccocus faecalis, staph aureus or coagulase negative infections following 10 days of appropriate intravenous antibiotic treatment (or 7 days post-surgery) – Class IIa recommendation.
Transoesophageal echocardiography should be performed in all those presenting with spondylodiscitis and/or septic arthritis with positive blood cultures for typical IE microorganisms as a class I indication.
There is a helpful section on coronary imaging prior to surgery for endocarditis, with a shift away from invasive angiography in all but the highest risk patients and a shift towards CT coronary angiography, especially in those with aortic valve vegetations.
Endocarditis represents a condition with a high mortality despite medical advances. The guidelines summarise the most up to date advances in this ever-changing field. The increasing use of cross-sectional imaging, the upgrade of the importance of the endocarditis team and the reduced reliance on parenteral antibiotics in simple cases represent important changes necessary to improving outcomes in this group of patients.
